Presenter: Dorothy Colby, Hale Kū‘ike Director of Community Engagement & Positive Approach to Care® Trainer
Date: 3/30/2022
Recording length: 1 hour, 15 minutes
Sponsors: Hale Kū‘ike and Catholic Charities Hawai‘i
Session:
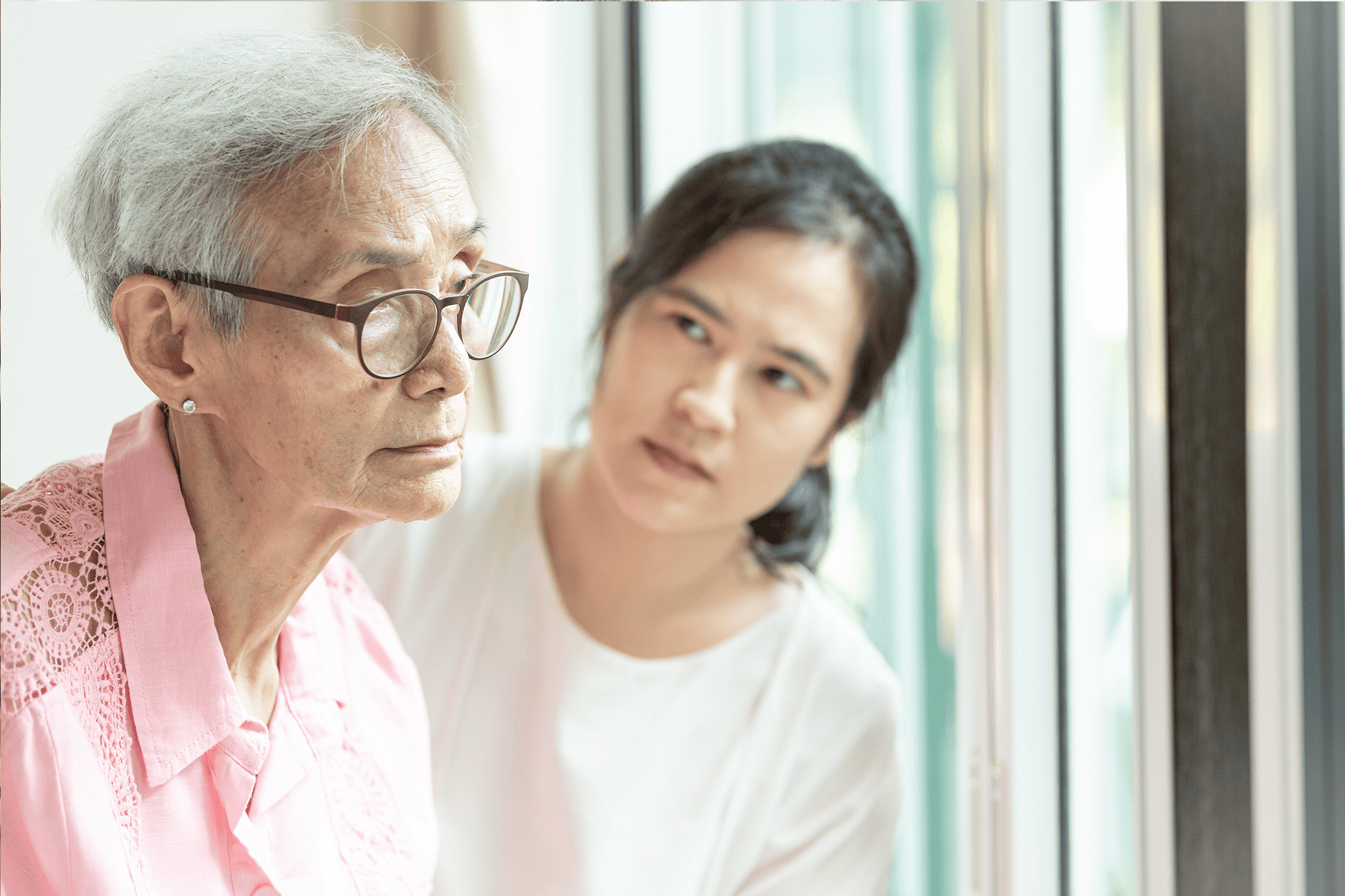
- Why do we keep arguing? Why can’t he find the bathroom? Why does she sleep all day? We find ourselves in challenging situations like these in dementia care every day.
- How can we take a step back and become curious, non-judgmental dementia detectives to find out why these challenging situations keep happening?
- We can learn how to be more effective and helpful in challenging situations by focusing our energy on the elements we CAN change vs. those we CANNOT
Uh-oh, that didn’t go the way I wanted it to! Uh-oh moments happen to us a lot when we are trying to support someone living with dementia. We are trying our best to give loving care, but still we find ourselves in endless arguments and stuck looking for solutions our challenges. If we can step back from these situations and look at them with curiosity and without judgement, we can learn from the experience. We want to turn these Uh-oh’s into Ah-ha’s
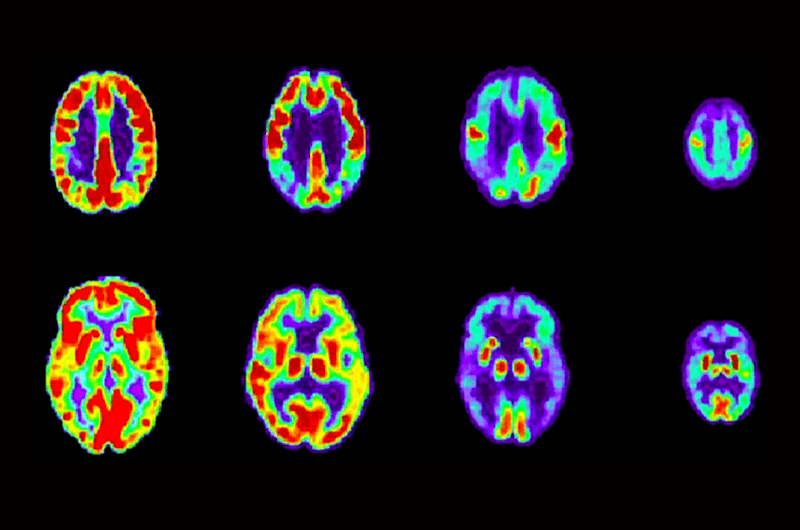
When we become dementia detectives, we learn about the brain changes that come with dementia so can start to understand the difference in how someone living with dementia perceives and interpret the world around them, including us, their care partners. We figure out how why loving offers of help might be interpreted as a threat to a changing brain. We work to see the environment through their eyes and understand why it might not be as easy to navigate as we think it is. The Positive Approach to Care®’s Six Pieces of the Puzzle tool can help us to look at all the factors that affect a person, and figuring out where we can make positive changes to help mitigate or prevent challenging situations.

Each of us as human beings is unique, with a unique personal history. We each have unique personal health and brain health statuses. These are the first three pieces of the puzzle that influence how we experience the world — The Person, Fitness/Health/Wellness, and Brain Change. Looking at these three pieces of the puzzle for yourself, which ones do you have influence to make positive changes? When we are young enough, the one we can make the most positive impact on the Fitness/Health/Wellness piece of the puzzle. Time is on our side.
Now thinking about those who are living with dementia, especially those who are elderly, how much influence do we have on these first three pieces of the puzzle? Who they have been does not change, though how that expresses itself may be different with brain change. We do not have as much influence over their Fitness/Health/Wellness piece as before. In general, because of advancing age and dementia, the person’s health goal has shifted curative measures to maintenance. We just want to try to have things not get worse, if we can help it. That third piece of the puzzle, Brain Change, is an important one to understand so that we can give better support. However, at this point in time, we cannot turn back the clock on dementia-related brain change.
The next three pieces of the puzzle are where we can focus our energy to make positive change — Stakeholders, Environment and Time. Everyone that touches a person living with dementia’s life is a stakeholder. You, other relatives, neighbors, the mail carrier, bus driver, healthcare professionals, they all influence how the person living with dementia experiences and responds to the world. The environment plays a big role in how successfully a person living with dementia moves through the world. Environments need to be friendly, familiar and forgiving of mistakes. The last piece of the puzzle is Time, how a person spends the hours of their day. Every person, whether they are living with dementia or not, needs meaningful engagement every day.
To learn more about challenging situations and how to move the needle on the Stakeholders, Environment and Time pieces of the puzzle, you can view our recorded webinar, “Challenging Situations in Dementia Care: Putting Together the Pieces of the Puzzle.” You can also download the workshop slide deck, GEMS printable poster, and PAC Resource Cards.
For more information about PAC, visit www.teepasnow.com.