Presenter: Dorothy Colby, Hale Kū‘ike Director of Community Engagement & Positive Approach to Care® Trainer
Date: 10/1/20
Recording length: 1 hour
Sponsors: Hale Kū‘ike and Catholic Charities Hawai‘i
Description:
- Dementia changes the sensory input systems. What does the world look, sound and feel like for someone living with dementia?
- Visual, verbal and touch processing are all affected. How can we get connected despite these changes?
- How can we become “care partners” instead of “care givers” in this dementia journey?
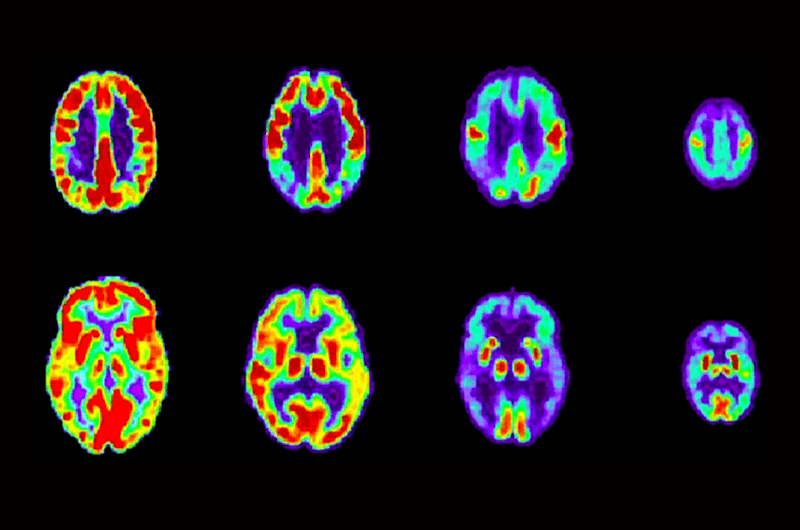
When we think about dementia changes, the focus is typically on memory changes. In fact, the entire brain and all its functions are affected by the diseases that cause dementia, not just the memory center. If we want to have effective communication and meaningful connections with someone living with dementia, we need to understand how other brain functions are affected.
As human beings, we want to see what is coming to feel safe. If there is a sound outside our vision, we turn and look. If we feel a touch we didn’t expect, we turn and look. When we are taken by surprise by something we see, hear or a touch, our fight-fright-flight response kicks in. Once we determine it is not a threat, then we can quickly start to relax and return to our calm baseline.
People living with dementia are no different. If they are taken by surprise, their fight-fright-flight response also kicks in, but because of their brain changes, it is much more challenging for them to process if something is not a threat and return to a calm state. If we do not want to kick off that fight-fright-flight response, we need to make sure we get a visual connection first before coming in to talk or touch.
The occipital lobe of the brain processes what we see in the world. We have a central field of active vision, and a wide peripheral awareness that is our safety vision. With all dementias, peripheral awareness narrows drastically, leaving a very narrow tunnel of active vision. The person simply is unaware of activity and objects outside that tunnel. It can be like looking at the world through a pair of binoculars. This often leads to trip and fall hazards and getting surprised by care partners touches.
The temporal lobes that process language are also affected. You might notice that a person living with dementia has trouble finding words or forming coherent sentences. This is paired with a change in comprehension. We talk and the person living with dementia hears us, but they cannot understand the content of your speech. Rhythm and musical abilities are preserved. So even though someone might not be able to speak, they can sing the words of old songs, prayers or poems they knew when they were young.
The Positive Physical Approach™ (PPA) and Hand Under Hand™ (HUH) techniques help us get connected in positive way. Their simple steps keep us in a person living with dementia’s narrow field of active vision, help us adjust our language to their changing language skills, and to get permission before touching. It is a dynamic assessment tool that allows us to build our relationship with the person we are trying to support, so that we can be “care partners” in everything we do. It helps us do “with” instead of “to” a person.
To learn more about dementia-related sensory changes, PPA, HUH and communication techniques, you can view our recorded webinar, “It’s All in Your Approach — Making Positive Connections.” You can also download the workshop slide deck and PAC Resource Cards.
For more information about PAC, visit www.teepasnow.com.